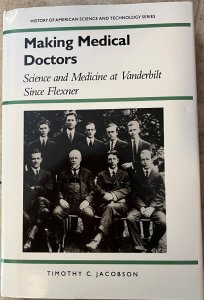
It often helps to look at history to understand the present. Vanderbilt Medical Center has a storied history, and fortunately, a few books preserve that story for the present. Timothy Jacobson’s Making Medical Doctors: Science and Medicine at Vanderbilt Since Flexner tells the story of Vanderbilt’s medical school since an important date. Although this book is about forty years old (and still available), it’s one of the most accessible records of the medical center’s founding. I’ll share some of that story here.
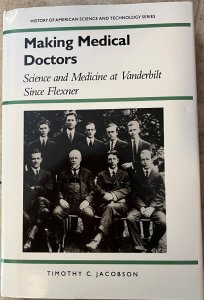
The title provokes the question: What exactly happened with Flexner? Even though the Flexner Report is over 100 years old, many working in medicine remain familiar with its name. Published in 1910, this report ultimately revolutionized the way the United States pursued medical education. It sought to make medical education follow the German model, then-recently pioneered in the US at Johns Hopkins. When implemented, it shut down many smaller medical schools that could not pursue scientific research, sadly including many schools focused on underserved populations. Instead, it recentered medical education around laboratory-based medicine, which it still is today. Thus far, this story is commonly shared.
Not as famous is the story of Vanderbilt’s central role in testing Abraham Flexner’s views. When the Flexner Report came out, many immediately doubted whether American medical education could adapt. They admired Johns Hopkins’ and the Germans’ work but questioned whether the entire nation could implement it. The report was too revolutionary for a grand scale, they said. In response, Flexner needed a test case to prove his ideas could apply broadly and looked for a good one for the next 15 years. He ultimately focused on a project to re-found Vanderbilt’s medical school, then an unnoteworthy institution in a stagnated region.
In 1925, Vanderbilt University was a private school focused on public service in the reconstructed South. Sixty years after the Civil War, the South was still recovering economically from war’s upheavals, and despite its initial endowment by tycoon Cornelius Vanderbilt, Vanderbilt tended to lag other Northern schools in quality. Without a standard-bearer for the new paradigm, medicine all over the South ran behind the times.
Vanderbilt Chancellor James Kirkland, Abraham Flexner, and Dean of Medicine G. Canby Robinson conspired to reboot the medical school into something much grander than had been previously run. It has operated since 1874 without much distinction, and the best Flexner could report was that it had “satisfactory laboratories” in many fields. However, it was enough for the visionary Kirkland to court Flexner to bring a new format. The three made an unusual group for the project: Kirkland was an ambitious Latin professor, Flexner an educator with no formal healthcare expertise, and only Robinson had a physician’s education at Johns Hopkins.
In 1925, Vanderbilt Medical School was re-founded to test Flexner’s ideas about a laboratory-based education. Before this date, the medical school did not stand out significantly from other Southern medical schools. However, Flexner, working with the Rockefeller Foundation’s General Education Board from 1912-1928, secured unique funding for Vanderbilt. At the time, large federal healthcare funding was not available, and no other institution received as big a largess from the Rockefeller family’s riches. With a religious penchant for good social deeds, the Rockefellers used their immense wealth from Standard Oil to advance noble ends across America all the way to Nashville.
Vanderbilt hired aggressively but wisely. The renewed Vanderbilt Medical School sought to integrate research and medical training intimately and attract nation-leading faculty to implement this new vision. Fortunately, dedicated scientific luminaries like Ernest Goodpasture signed up for the grand experiment. Vanderbilt capitalized on the spirit of the age in that, like Johns Hopkins and its German forebears, it integrated the clinic and the lab intimately. Unlike these others, it did so in a region that was not as economically vibrant – an impressive feat to reconstruct a still-divided nation. It proved that with proper funding and leadership, a successful, research-driven medical school was possible anywhere. The Flexner Report’s ambitions were proven feasible even in the recovering South. Eventually, they were implemented nationwide.
(For more information about the Flexner Report’s broader impact on American medicine, I recommend the treatment in The Social Transformation of American Medicine by Paul Starr (1982) on pages 116-127. The book won a Pulitzer Prize in 1984 and is a gem to understand the American medical system’s history. Another treatment is available at Duffy TP. The Flexner Report–100 years later. Yale J Biol Med. 2011 Sep;84(3):269-76. PMID: 21966046; PMCID: PMC3178858.)
Then truly innovative, attendings, students, and residents could roam freely between labs and clinics at Vanderbilt in an almost seamless manner. Goodpasture provides a good example of its value. As a pathologist, he famously invented a way to mass produce viral material in egg yolks. This was a key step to mass producing viral material to disseminate vaccines to the wider population. By integrating the clinical question of supplying vaccines with a laboratory method, he demonstrated the value of close-knit relationships between the clinic and the lab. Not many other places in the world could have produced such an innovation.
Before an era of big government grants, these scientists spent their days quietly bringing the lab to patients and patient care into lab work. Using luminaries like Johns Hopkins’ William Osler as a launch pad, they showed that science could broadly meet society’s needs for medical care, starting in Nashville.
After World War II, many medical centers grew along Vanderbilt’s model with increased federal biomedical research funding. Unlike other centers, however, Vanderbilt’s administration deliberately aimed to keep alive the dream of major research advances. Many institutions used federal funds to provide jobs for regional facilities; as Jacobson details, Vanderbilt sought to maintain its initial vision of integrating labs and the clinics in novel ways. Its identity remains, in no small part, to integrate and translate research and clinical advancements.
Jacobson’s book details many more ebbs and flows of Vanderbilt’s journey until the book’s publication in 1987. With stories like these, he illustrates that education, research, and service served as historic foundations still directing its course. Since its re-founding, Vanderbilt never intended to be merely another medical center, but instead to lead healthcare projects from bench to bedside and back way before that catchphrase was ever dreamed of. Its students impacted the entire southern region with a curious, scientific approach to medical care. This history can guide our biomedical community to continue to imagine big for the nation’s and world’s patient care today.
Making Medical Doctors: Science and Medicine at Vanderbilt Since Flexner
By Timothy C. Jacobson
Copyright © 1987
The University of Alabama Press
ISBN13 9780817303150
Page Count: 349